
'We have to move from strategy to action': Tackling Health Inequalities 2025
On Tuesday 28 January 2025 we held our third annual Tackling Health Inequalities conference in partnership with NHS England. It was a truly thought-provoking day, filled with inspired talk and a universal willingness to turn conversation into tangible action. Thank you so much to all the speakers and to those who attended the events.
Here are some of the highlights from the day:
Tackling Health Inequalities, to achieve the health mission
The day was filled with actionable insight, including Director of Healthcare Inequalities at NHS Professor Bola Owolabi’s closing remarks: “There is a bridge between achieving the health mission and the economic health mission and that bridge is to narrow the health inequalities gap. And I say that on the basis that the burden of ill health is formed disproportionately, and so our most disadvantaged communities are bearing a greater burden of ill health, and that ill health is driving economic inactivity. So, it stands to reason that… if we don’t drive our resources, our investments, our efforts in the direction of those underserved communities, then actually we’re not going to achieve the health mission and by extension we will not achieve the economic growth mission.”

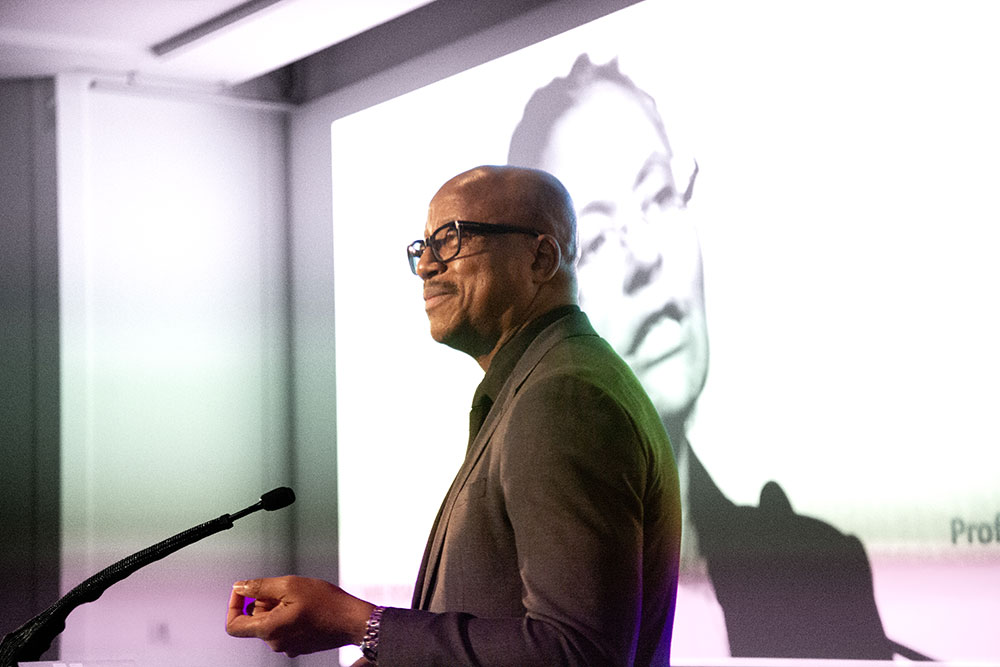
Professor Bola Owolabi addresses the audience at our third annual Tackling Health Inequalities conference
The future of the NHS
Sally Warren, Director General of the 10 Year Health Plan at the Department of Health and Social Care, spoke about how their team is currently engaging with the public and NHS staff in the largest ever conversation about the future of the NHS. She highlighted the common threads to come out of the conversations that they have had so far, noting that patients and staff are proud of the NHS, but currently the basics are not being done right. She went on to talk about the vision working groups, tasked with making a more equitable NHS a reality. The groups have centred their work around the statement of “I am treated in a fair and inclusive way, irrespective of who I am”. The themes to emerge to help towards this goal are:
- Increasing focus on the most deprived areas and communities where health inequalities are greatest
- Involving organisations from a wide range of communities to better meet patient needs
- Mitigating digital exclusion, ensuring services are accessible to all
- An NHS that is inquisitive about those it is caring for
- Trust is key in tackling health inequalities
- A shift in power to patients and communities
Racism and health inequalities
Professor Kevin Fenton CBE, President at the Faculty of Public Health spoke about health inequalities and racism. He started by setting the scene, so we could understand the depths of the problem we are facing: “We are seeing an increase in the number of people living with chronic conditions, it is projected that this will be the case of 1 in 5 adults in England by 2040. We also see that those in the least deprived areas of the UK can expect to live 70 years in good health, compared to 50 years for those in the most deprived areas.” He goes on to discuss the effect structural racism in healthcare has on ethnic minorities: "people experiencing structural discrimination and racism are much more likely to die earlier, they're much more likely to develop a range of mental health and physical health conditions, which results in a greater burden on health and care systems. They're much less likely to trust and have confidence in the healthcare system and therefore less likely to come forward for vaccinations and screening programmes, that protect them and their families."
“How do you have a universal service, but that also recognises people individual and cultural backgrounds? This is why we need meetings like today.” Professor Kevin Fenton CBE
Poverty and health inequalities
Professor Maggie Rae CBE, President of the RSM's Epidemiology and Public Health Section, spoke to how poverty being the root cause of ill health is a major public crisis and the importance of children having the best start in life in order to escape poverty: “[school readiness] is a national crisis. If we were working in emergency planning, this would be declared a major incident. So, poor children are costing us an absolute fortune… the work we have been doing… has actually been demonstrating ‘if you invest in this, you will save money’. Because you really need to understand what is happening to children who aren’t ready for school, and the numbers are going up and up, and how teachers are going to be able to cope with all of that added pressure and there’s a whole generation of children whose life chances are being stolen. The simple fact of having good language and good communication, if you haven’t got that as you go through the first 1000 days and then onto nursey and school you will fail. And what’s the number one best route out of poverty? Good education and a good job.”
The experience of health inequalities for working people and communities
In our first panel discussion we were joined by Duleep Allirajah, Chief Executive at the Richmond Group of Charities, Kevin Garrod, Anchor Programme Manager - Local Value Lead, at Mid and South Essex NHS Foundation Trust and Andrew Fenton, Director - Population Health and Health Inequalities at NHS South Central and West. There was discussion around how it is increasingly difficult for some members of the public to hold down work whilst attending NHS appointments. An example was provided by Mr Allirajah, from a report on ‘what people with multiple health conditions have to say about health equity’, to demonstrate the point: “The worst year I had for appointments… I had 68 appointments, different departments, different check-ups, that was doctors, GPs, hospitals and diabetes checks, eye checks and everything else. I had to give up work because of it.”
The role of clinical trials
Executive Director, Medical Affairs and Strategic Partnerships at ABPI, Dr Amit Aggarwal opened up discussions about the valuable role industry clinical trials have to play in individual patient outcomes but have “historically failed to engage a diverse group of participants from different ethnic and racial backgrounds.” He noted that “creating more supportive environments for a diverse range of individuals to participate in clinical trials is a critical step in achieving health equity.” In order to do this, we need to get a “clear view of how people currently think about clinical trials [to] help identify what steps need to be taken to make this a reality”. He explained that ethnic minorities respondents are not just less likely to be willing to take part in a clinical trial compared to white respondents, but also less likely to be asked to take part. He went on to say, “fear and mistrust play a large role in preventing ethnic minorities in the UK from participating in clinical trials.” John James OBE, Chief Executive Officer at The Sickle Cell Society spoke of one step forward in making clinical trials more inclusive in our second fireside talk on research: “[we need to make] clinical trials and research mandatory for inclusion and diversity… and that’s a message also for industry.”

Our second Fireside chat, chaired by RSM President Professor Gillian Leng CBE
Turning research into action
Also, in this fireside chat we had Professor Lucy Chappell, Chief Scientific Adviser at the Department of Health and Social Care, Professor Dame Lesley Regan DBE, Professor of Obstetrics and Gynaecology at Imperial College London and Jason Yiannikkou Director, Systems, Integration and Reform Team at Department of Health and Social Care. The importance of collecting both qualitative and quantitative data was discussed in ensuring patients' lived experiences are captured. As well as the empirical data to back up those lived experiences. The sentiment of acting on data was shared by all but summed up by Professor Chappell: “we have to move from strategy to delivery and action.”

"We need to focus on what's strong and not what's wrong" Cormac Russell
How community can be the source of good health
We ended the day with Cormac Russell’s talk on ‘The neighbourhood as a primary unit of health creation’. His talk was filled with powerful and inspiring anecdotes and actions, on how we can build stronger communities and trust, and how in doing this, neighbourhoods can become individuals’ primary source of good health. He ended his talk by saying; “if we start with what’s strong not with what’s wrong in communities, we’re going to discover all kinds of possibilities that are currently languishing. If we also are prepared to start with a discovery rather than delivery mentality, I think we’ll discover a whole range of health creation capabilities that are currently not available to us.”
